ECZEMAS AND DRUG HYPERSENSITIVITY
3.3
Mechanisms of contact dermatitis and eczema
Three major types of dermatitis or eczema are distinguished: Allergic contact dermatitis, irritant contact dermatitis, and atopic dermatitis. The most common external cause of contact dermatitis is contact with mild toxic agents or irritants (eg water and soaps), causing irritant contact dermatitis. Allergic contact dermatitis is less common than irritant contact dermatitis and reflects a contact allergy to a specific substance, such as nickel, rubber components, or perfumes (fragrances). Atopic dermatitis has several causes – some exogenous and some endogenous based on a genetic background.
Eczema belong to the most common diseases in dermatology. From a pathophysiological point of view, an eczema is a non-infectious, cell-mediated inflammation of the superficial skin layers. It may develop spontaneously, however, often exogenous triggers are important. We distinguish three common subtypes: allergic or irritant contact eczema and atopic dermatitis. The two subtypes of contact eczema may differ in their appearance, localisation and in their mechanisms and causes. 75 to 80% of cases are caused by irritants, 20 to 25% by contact allergens.
Allergic contact dermatitis
Allergic dermatitis or eczema is triggered by contact allergens. Contact allergens are typically small molecules with a low molecular weight, so-called haptens. The immunological mechanism behind allergic contact dermatitis corresponds to a delayed type (or type IV according to Coombs and Gell) hypersensitivity reaction.
[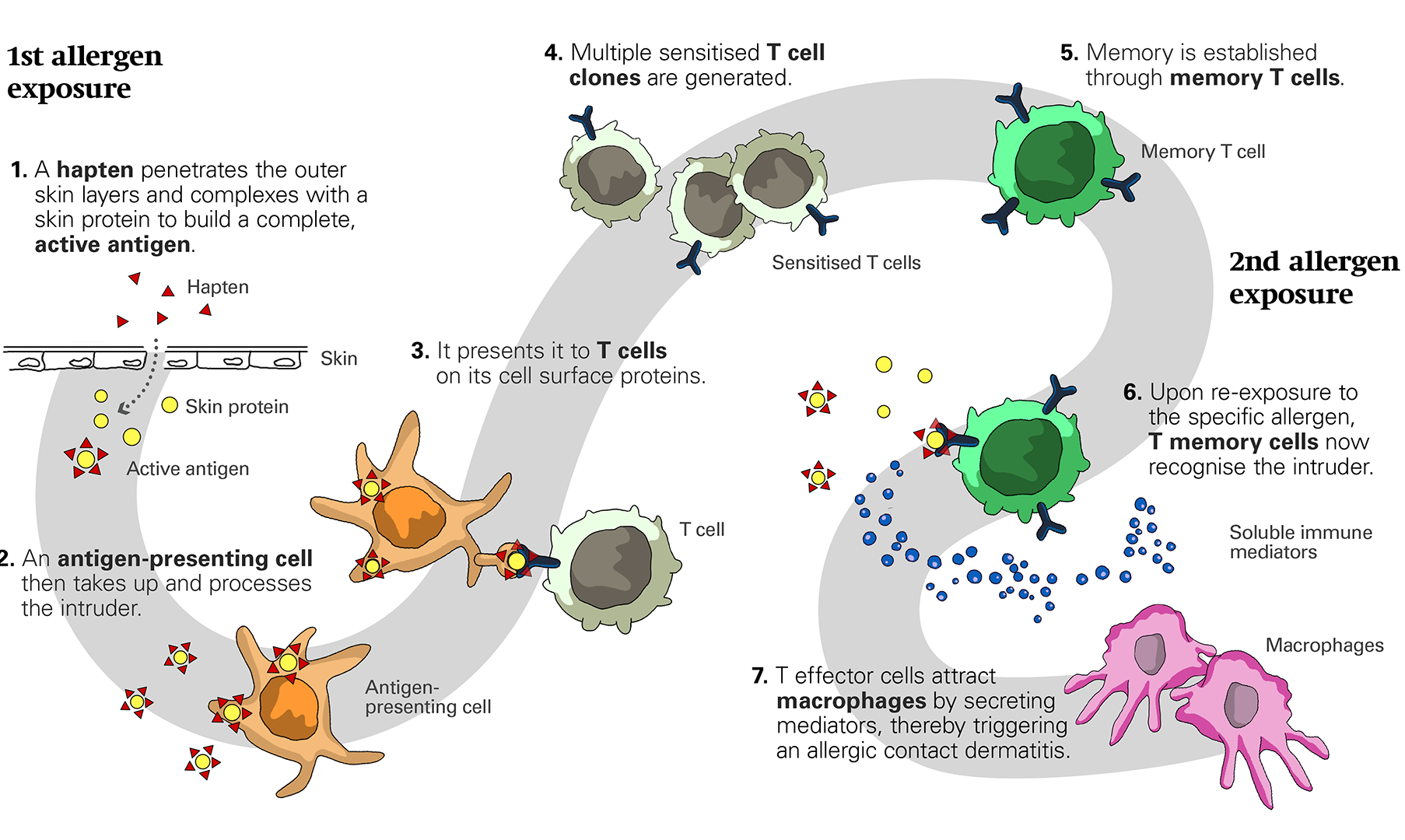
Mechanisms of allergic contact dermatitis and eczema. (click to enlarge)
First allergen exposure:
As in immediate type allergic reactions, at a first allergen exposure the body may become sensitized.
1. A hapten penetrates the outer skin layers and complexes eg with a skin protein to build a complete allergen that can be recognized by the immune cells.
2. An antigen-presenting cell (APC) then takes up and processes the intruder.
3. It presents it to T cells on its cell surface proteins. These proteins are called major histocompatibility complex (MHC) or human leukocyte antigen (HLA) molecules and represent an identification system present on all body cells (except on red blood cells and platelets) allowing to distinguish self from foreign.
4. This presentation leads to the proliferation of the T cell. In this process multiple T cells, a clone, specific for this antigen, are generated.
5. Memory is established through memory T cells which recognize the specific antigen faster upon later re-exposure.
Second allergen exposure:
Only at an ongoing or subsequent exposure to the same allergen, allergic symptoms occur.
6. Upon re-exposure to the specific allergen, T memory cells now rapidly recognize the intruder.
7. T effector cells attract macrophages by secreting mediators. Within one to two days, an inflammatory response resulting in an allergic contact dermatitis is triggered.
Some haptens (eg as nickel) may directly bind to the MHC molecules of APCs and thereby easily induce sensitization. Some fragrances (eg limonene) are so-called prehaptens, which spontaneously turn into allergenic molecules if exposed to oxygen. Finally, prohaptens (eg para-phenylenediamine) are substances that are metabolized into the allergenic compound within the patient’s skin.
Irritant contact dermatitis
In irritant (non-allergic) contact dermatitis, the skin barrier is primarily disturbed, resulting in inflammation mediated by innate immune mechanisms. Common irritants include water, soaps, detergents, cold temperature, mild acids and alkali, as well as ultraviolet radiation. At the affected site, the skin burns, turns red, dry, and finally scales; painful fissures and crevasses may arise. It is mainly confined to the site of exposure to the irritants.
Atopic dermatitis
Atopic dermatitis, on the other hand, has a strong genetic background and typically occurs for the first time during early childhood. It may be triggered by irritants, food allergens, and microbial antigens. Indeed, due to an impaired skin barrier, patients with atopic dermatitis are more sensitive to irritants (eg frequent washing, soap use, and cold dry weather). In some patients with atopic dermatitis, the skin condition may be aggravated by food allergens. Bacterial or fungal overgrowth may trigger inflammation and complicate the skin condition through additional infections. Finally, the frequent use of topical medications and care products may result in sensitization to some of its components. An allergic contact dermatitis may be superimposed onto the atopic dermatitis, further aggravating the skin inflammation.
License
University of Basel
